Stress and blood sugar are more intertwined than most people realize, creating a complex biological dance that affects millions worldwide daily. 🧬
In our fast-paced modern world, stress has become an unwelcome companion for many individuals. Whether it’s work deadlines, family responsibilities, financial pressures, or health concerns, stress manifests in numerous ways throughout our bodies. One of the most significant yet often overlooked impacts of stress involves our blood sugar levels and glucose regulation systems.
Understanding the intricate relationship between psychological stress and blood glucose variability is crucial for anyone interested in metabolic health, diabetes management, or overall wellness. This connection affects not only people with diabetes but also those without any diagnosed metabolic conditions, making it a universal health concern worth exploring in depth.
The Biological Foundation: How Your Body Responds to Stress 💪
When you encounter a stressful situation, your body initiates an ancient survival mechanism known as the “fight or flight” response. This physiological reaction, orchestrated by your nervous system and endocrine glands, was designed to help our ancestors escape immediate physical dangers.
During this stress response, your adrenal glands release several hormones, primarily cortisol and adrenaline (epinephrine). These stress hormones trigger a cascade of metabolic changes throughout your body, with one primary goal: providing immediate energy to deal with the perceived threat.
Part of this energy mobilization involves releasing stored glucose from your liver into your bloodstream. Your body essentially floods your system with readily available fuel, anticipating that you’ll need it for intense physical activity. This mechanism served our ancestors well when fleeing from predators or hunting for food.
The Modern Stress Paradox
The challenge in contemporary life is that our stress rarely requires physical exertion. When you’re stressed about a work presentation, stuck in traffic, or worried about paying bills, your body still releases glucose into your bloodstream—but you’re not burning it through physical activity. This creates a situation where blood sugar rises without the corresponding expenditure that would naturally bring it back down.
This mismatch between our biological programming and modern lifestyle creates significant metabolic consequences that can affect blood sugar stability over both short and long time periods.
The Cortisol-Glucose Connection Explained 🔬
Cortisol, often called the “stress hormone,” plays a particularly important role in blood sugar regulation. This hormone doesn’t just trigger a one-time glucose release; it fundamentally alters how your body processes and stores energy.
When cortisol levels remain elevated due to chronic stress, several metabolic changes occur:
- Increased gluconeogenesis: Your liver produces more glucose from non-carbohydrate sources like amino acids and fats
- Reduced insulin sensitivity: Your cells become less responsive to insulin’s signals to absorb glucose from the bloodstream
- Decreased glucose uptake: Muscle and fat cells absorb less glucose, leaving more circulating in your blood
- Increased appetite: Particularly for high-calorie, sugary foods that can further elevate blood glucose
- Altered fat distribution: More fat storage around the abdomen, which itself contributes to insulin resistance
These changes create a perfect storm for blood sugar variability, with levels swinging higher than normal and taking longer to return to baseline after eating or during stressful events.
Acute Stress vs. Chronic Stress: Different Impacts on Blood Sugar 📊
Not all stress affects your blood sugar in the same way. The duration and intensity of stress play crucial roles in determining its metabolic impact.
Acute Stress Effects
Short-term, intense stress—like narrowly avoiding a car accident or delivering an important presentation—causes immediate blood sugar spikes. For most healthy individuals, these temporary elevations resolve quickly once the stressor passes, typically within 30 to 60 minutes.
However, people with diabetes or prediabetes may experience more pronounced spikes and longer recovery times. Their already compromised glucose regulation systems struggle more significantly with the additional burden of stress hormones.
Chronic Stress Complications
Ongoing, persistent stress creates far more problematic patterns. When your body remains in a semi-constant state of stress response, cortisol and other stress hormones stay elevated for extended periods. This chronic elevation fundamentally disrupts your metabolic homeostasis.
Research has shown that chronic stress contributes to increased fasting blood glucose levels, higher HbA1c readings (a marker of long-term glucose control), and greater glucose variability throughout the day. This variability—the ups and downs of blood sugar rather than just the average level—is increasingly recognized as an independent risk factor for complications.
The Hidden Stressors: Beyond the Obvious Triggers ⚠️
While we often think of stress in psychological terms—work pressure, relationship conflicts, or financial worries—many other factors trigger the same physiological stress response that affects blood sugar.
Physical stressors that impact glucose regulation include:
- Inadequate or poor-quality sleep (even one night of sleep deprivation)
- Illness or infection, as your immune system mobilizes resources
- Chronic pain conditions that keep your nervous system activated
- Excessive exercise or overtraining without adequate recovery
- Caffeine consumption, particularly in high amounts or late in the day
- Dehydration, which concentrates glucose in your bloodstream
Environmental and lifestyle stressors also contribute to this burden. Irregular meal timing, skipping meals, and then overeating create their own form of metabolic stress that compounds psychological stress effects on blood sugar.
The Vicious Cycle: When Blood Sugar Fluctuations Create More Stress 🔄
The relationship between stress and blood sugar isn’t one-directional. Blood glucose variability itself can trigger stress responses, creating a self-perpetuating cycle that becomes increasingly difficult to break.
When blood sugar drops too low (hypoglycemia), your body perceives this as a survival threat. This triggers the release of stress hormones including adrenaline and cortisol to raise glucose levels back up. The symptoms of this counter-regulatory response—shakiness, sweating, anxiety, rapid heartbeat—are virtually identical to anxiety symptoms.
Similarly, when blood sugar remains elevated, it can cause symptoms like fatigue, difficulty concentrating, and irritability—all of which increase perceived stress and reduce your capacity to cope with challenges effectively.
This bidirectional relationship means that managing either stress or blood sugar can positively impact the other, offering multiple intervention points for improving overall metabolic health.
Stress, Sleep, and Blood Sugar: The Triangle of Metabolic Health 😴
Sleep represents a critical but often underappreciated factor in the stress-blood sugar connection. Poor sleep simultaneously increases stress and disrupts glucose metabolism through multiple mechanisms.
When you don’t get adequate sleep, cortisol patterns become dysregulated. Normally, cortisol follows a daily rhythm, highest in the morning and declining throughout the day. Sleep deprivation flattens and elevates this curve, keeping cortisol higher throughout the day and night.
Sleep restriction also increases insulin resistance, meaning your body needs more insulin to process the same amount of glucose. Studies have shown that even a single night of partial sleep loss can reduce insulin sensitivity by up to 25% the following day.
Additionally, poor sleep increases appetite-stimulating hormones and decreases satiety signals, leading to increased food intake—particularly of high-carbohydrate comfort foods that cause more dramatic blood sugar fluctuations.
Practical Strategies: Managing Stress to Stabilize Blood Sugar 🎯
Understanding the connection between stress and blood glucose variability is valuable, but implementing practical strategies to manage this relationship is where real health improvements occur.
Mind-Body Techniques That Work
Research consistently demonstrates that stress-reduction practices can improve blood sugar control. Meditation, particularly mindfulness-based stress reduction (MBSR), has been shown in multiple studies to reduce HbA1c levels and improve glucose variability in people with diabetes.
Deep breathing exercises activate your parasympathetic nervous system—the “rest and digest” counterpart to the stress response. Even brief breathing practices, done consistently, can lower cortisol levels and improve insulin sensitivity over time.
Yoga combines physical movement, breath work, and meditation, offering a comprehensive approach to stress management that addresses multiple pathways affecting blood sugar regulation.
Physical Activity: The Dual-Action Solution
Regular physical activity serves as both a stress management tool and a direct blood sugar regulator. Exercise reduces stress hormones, improves insulin sensitivity, and helps muscles absorb glucose without requiring insulin.
The key is finding the right balance. While moderate exercise improves glucose regulation, excessive high-intensity exercise without adequate recovery can actually increase stress hormones and temporarily raise blood sugar. For most people, a combination of moderate aerobic activity and strength training provides optimal benefits.
Even brief movement breaks throughout the day—particularly after meals—can significantly reduce blood sugar spikes and lower overall glucose variability.
Nutrition Strategies for Stress and Blood Sugar
What you eat affects both stress resilience and blood glucose stability. Complex carbohydrates paired with protein and healthy fats create more stable blood sugar patterns than simple carbohydrates alone.
Certain nutrients specifically support stress response systems. Magnesium, often depleted during periods of high stress, plays important roles in both glucose metabolism and nervous system regulation. B-vitamins support energy production and neurotransmitter synthesis. Omega-3 fatty acids help modulate inflammation and cortisol responses.
Consistent meal timing also helps regulate both stress hormones and blood glucose. Skipping meals creates physical stress that triggers cortisol release and can lead to reactive overeating and blood sugar swings.
Monitoring and Awareness: Knowledge as a Management Tool 📱
Awareness of your personal stress-glucose patterns can be incredibly empowering. Many people discover specific triggers they hadn’t previously recognized once they start paying attention to the connection.
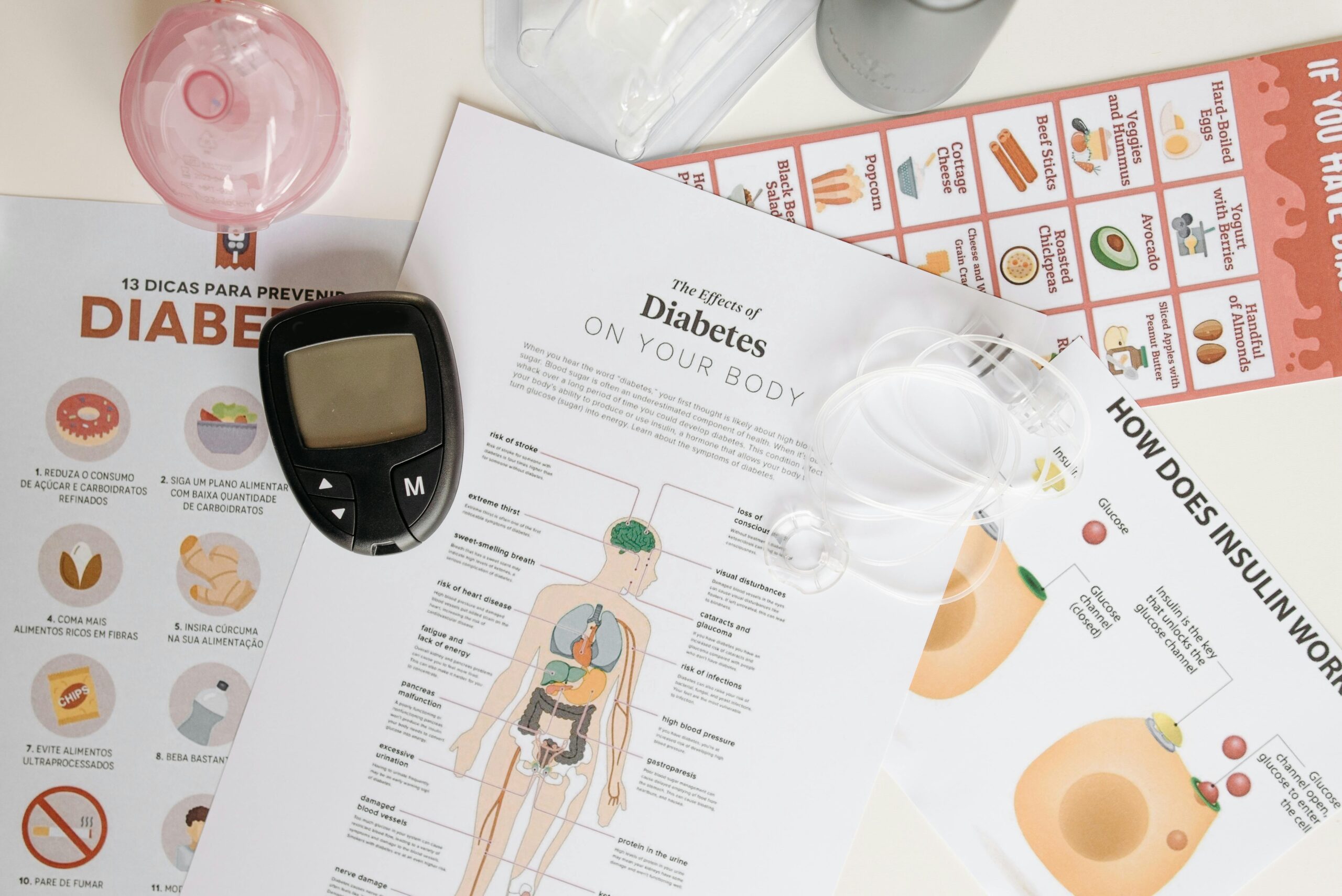
Continuous glucose monitors (CGMs), once reserved primarily for people with diabetes, are increasingly being used by individuals interested in understanding their metabolic health. These devices reveal real-time glucose responses to various stressors, foods, activities, and sleep patterns.
Keeping a simple log that tracks stress levels alongside blood glucose readings (if you monitor) can reveal patterns. You might discover that your Monday morning meetings consistently spike your blood sugar, or that you sleep poorly creates higher fasting glucose the next day.
When Professional Help Makes Sense 👨⚕️
While lifestyle strategies form the foundation of managing the stress-blood sugar connection, some situations warrant professional guidance.
If you’re experiencing chronic stress that you can’t manage through self-care strategies, mental health professionals can provide evidence-based treatments like cognitive-behavioral therapy (CBT), which has been shown to improve both stress management and glycemic control.
For individuals with diabetes or prediabetes, working with an endocrinologist or certified diabetes educator can help optimize medication management while implementing stress-reduction strategies. Sometimes medication adjustments are needed during particularly stressful periods.
Registered dietitians, particularly those specializing in diabetes care, can create personalized nutrition plans that address both blood sugar stability and stress-related eating patterns.
Building Resilience: Long-Term Metabolic Health 🌱
Managing the stress-blood sugar connection isn’t about achieving perfection or eliminating all stress from your life—an impossible goal. Instead, it’s about building resilience: the capacity to maintain metabolic stability despite life’s inevitable challenges.
Resilience develops through consistent practices rather than occasional interventions. Small, sustainable changes maintained over time create more significant impacts than dramatic short-term efforts that can’t be sustained.
This might mean committing to ten minutes of daily meditation rather than occasionally attending hour-long yoga classes. It could involve taking three ten-minute walks daily instead of planning elaborate workout routines you rarely complete. The key is consistency and sustainability.
Building social connections also enhances resilience. Strong relationships buffer stress responses and provide practical and emotional support during challenging times. Social isolation, conversely, acts as a chronic stressor that negatively impacts both mental health and metabolic function.

Transforming Understanding Into Action 🚀
The connection between stress and blood sugar variability represents both a challenge and an opportunity. While stress can certainly disrupt glucose regulation, understanding this relationship provides multiple pathways for intervention and improvement.
Every stress management technique you implement doesn’t just reduce psychological strain—it directly benefits your metabolic health. Every blood sugar stabilization strategy you adopt doesn’t just improve glucose control—it enhances your stress resilience.
Start by choosing one or two strategies that feel most manageable and relevant to your life. Perhaps it’s establishing a consistent sleep schedule, taking a brief walk after dinner, or practicing five minutes of deep breathing before bed. Implement these consistently for several weeks, then add additional practices as these become habitual.
Remember that managing the stress-blood sugar connection is a journey rather than a destination. Progress may not always be linear, and that’s perfectly normal. What matters is the overall trajectory and your commitment to supporting your body’s metabolic health through manageable, sustainable practices.
By recognizing stress as a significant factor in blood sugar variability and implementing targeted strategies to address this connection, you take powerful steps toward better metabolic health, improved energy, enhanced mood stability, and reduced risk of long-term complications. Your body’s stress and glucose systems are intimately connected—working with this connection rather than against it creates the foundation for lasting health improvements.
Toni Santos is a metabolic rhythm researcher and circadian nutrition specialist focusing on the study of blood-sugar oscillation patterns, clock-aligned eating frameworks, and the physiological languages embedded in energy dynamics and restorative sleep. Through an interdisciplinary and data-focused lens, Toni investigates how humanity can decode metabolic balance, vitality, and recovery into the nutritional world — across rhythms, cycles, and optimized routines. His work is grounded in a fascination with nutrition not only as fuel, but as carriers of temporal meaning. From blood-sugar rhythm tracking to energy-curve optimization and clock-aligned meal cycles, Toni uncovers the metabolic and temporal tools through which individuals preserve their relationship with the circadian unknown. With a background in metabolic analytics and circadian nutrition science, Toni blends rhythm analysis with biological research to reveal how meals were used to shape vitality, transmit energy, and encode restorative knowledge. As the creative mind behind montyrax, Toni curates illustrated metabolic maps, speculative rhythm studies, and temporal interpretations that revive the deep biological ties between nutrition, circadian cycles, and forgotten metabolic science. His work is a tribute to: The lost metabolic wisdom of Blood-Sugar Rhythm Tracking Practices The guarded rituals of Clock-Aligned and Circadian Meal Cultivation The physiological presence of Energy-Curve Optimization Rhythms The layered temporal language of Sleep-Compatible Nutrition and Cycles Whether you're a metabolic historian, circadian researcher, or curious gatherer of forgotten rhythm wisdom, Toni invites you to explore the hidden roots of nutritional knowledge — one cycle, one curve, one rhythm at a time.