Blood sugar management remains one of the most misunderstood aspects of health, with myths often overshadowing scientific facts and preventing people from making informed decisions.
In today’s information-saturated world, separating fact from fiction about blood glucose has become increasingly challenging. Social media influencers, well-meaning friends, and even some healthcare providers sometimes perpetuate misconceptions that can lead to confusion, unnecessary anxiety, or worse—improper management of this critical health marker. Whether you’re living with diabetes, prediabetes, or simply trying to optimize your metabolic health, understanding what’s true and what’s myth can dramatically impact your wellbeing.
This comprehensive guide cuts through the noise to address the most persistent myths surrounding blood sugar stability, providing evidence-based insights that empower you to take control of your metabolic health with confidence and clarity. 🎯
The Foundation: Understanding Blood Sugar Basics
Before diving into specific myths, it’s essential to establish a foundational understanding of how blood sugar actually works. Your blood glucose levels naturally fluctuate throughout the day in response to various factors including food intake, physical activity, stress, sleep quality, and hormonal changes.
The body maintains these levels through a sophisticated system involving insulin and glucagon—hormones produced by the pancreas. When functioning optimally, this system keeps blood sugar within a healthy range, typically between 70-100 mg/dL when fasting and below 140 mg/dL two hours after eating.
Problems arise when this regulatory system becomes impaired, leading to conditions like insulin resistance, prediabetes, or diabetes. Understanding this mechanism helps contextualize why so many myths persist—blood sugar regulation is genuinely complex, making oversimplified explanations tempting but often misleading.
Myth #1: All Carbohydrates Are Created Equal 🍞
One of the most pervasive misconceptions is that all carbohydrates affect blood sugar identically. This oversimplification ignores the fundamental differences between simple and complex carbohydrates, as well as the crucial role of fiber, protein, and fat in moderating glucose response.
The glycemic index (GI) and glycemic load (GL) demonstrate scientifically that carbohydrate sources produce vastly different blood sugar responses. A slice of white bread spikes glucose rapidly, while the same amount of carbohydrates from lentils produces a gradual, sustained release.
The distinction matters immensely for blood sugar stability. Complex carbohydrates paired with fiber slow digestion, preventing the dramatic spikes and crashes associated with refined carbs. Additionally, combining carbohydrates with protein and healthy fats further moderates the glycemic response—a strategy known as macronutrient balancing.
The Reality of Carbohydrate Quality
Research consistently shows that whole food sources of carbohydrates—vegetables, legumes, whole grains, and fruits—contain nutrients and fiber that processed carbohydrates lack. These components don’t just slow absorption; they also feed beneficial gut bacteria, reduce inflammation, and provide essential vitamins and minerals.
Rather than fearing all carbs, focus on quality and context. A sweet potato with dinner alongside protein and vegetables creates an entirely different metabolic response than a sugary dessert consumed alone on an empty stomach.
Myth #2: You Must Eliminate Sugar Completely
The “sugar is poison” narrative has gained tremendous traction, leading many to believe that any amount of sugar will derail blood sugar control. While excessive sugar consumption undeniably contributes to metabolic problems, the complete elimination approach often backfires psychologically and isn’t supported by moderate, evidence-based recommendations.
Your body doesn’t distinguish between “natural” and “added” sugars at the molecular level—glucose is glucose, fructose is fructose. However, the package matters enormously. An apple contains sugar, but also fiber, polyphenols, vitamins, and water that modulate its impact. Table sugar or high-fructose corn syrup provides calories without these beneficial compounds.
Research indicates that occasional, modest amounts of added sugar within an otherwise balanced diet don’t significantly impair metabolic health in most people. The key lies in quantity, frequency, and overall dietary pattern rather than absolute prohibition.
Finding Balance Without Restriction
Sustainable blood sugar management incorporates flexibility rather than rigid rules. A small piece of dark chocolate after a balanced meal has minimal impact on glucose levels and may actually improve dietary adherence by preventing feelings of deprivation that lead to binge eating.
The 80/20 principle applies well here—when 80% of your diet consists of whole, minimally processed foods, the remaining 20% can include treats without compromising metabolic health. This approach proves far more sustainable than perfectionist elimination that often ends in cycles of restriction and overconsumption.
Myth #3: Blood Sugar Concerns Only Matter for Diabetics
Perhaps the most dangerous myth is the belief that blood sugar stability only concerns people with diagnosed diabetes. In reality, metabolic health exists on a continuum, and blood sugar dysregulation begins long before diabetes diagnosis. 📊
Insulin resistance—the condition preceding type 2 diabetes—affects an estimated 40% of American adults, many completely unaware of their status. During this stage, blood sugar may still appear normal on standard tests because the pancreas compensates by producing more insulin. However, this compensation comes at a cost: increased inflammation, elevated triglycerides, weight gain (especially abdominal), and increased cardiovascular disease risk.
Furthermore, blood sugar instability affects everyone’s energy, mood, cognitive function, and appetite regulation. The mid-afternoon energy crash, brain fog, intense cravings, and irritability when hungry often stem from blood sugar fluctuations rather than character flaws or lack of willpower.
Prevention Beats Treatment Every Time
Waiting until diabetes diagnosis to address blood sugar means intervening after significant metabolic damage has occurred. Prediabetes and even pre-prediabetic insulin resistance are largely reversible through lifestyle modifications—diet, exercise, sleep optimization, and stress management.
Everyone benefits from blood sugar awareness regardless of diabetic status. Stable glucose levels enhance mental clarity, sustain energy throughout the day, improve athletic performance, support healthy weight management, and reduce long-term disease risk.
Myth #4: Exercise Always Lowers Blood Sugar Immediately
While physical activity generally improves glucose control and insulin sensitivity, the relationship between exercise and immediate blood sugar levels is more nuanced than commonly believed. Many people discover through continuous glucose monitoring that their blood sugar actually rises during or immediately after certain types of exercise—a phenomenon that can cause unnecessary concern.
High-intensity exercise triggers the release of stress hormones like cortisol and adrenaline, which signal the liver to release stored glucose for energy. This physiological response is completely normal and beneficial, even though it temporarily elevates blood sugar. The glucose gets utilized by working muscles and levels typically normalize within 1-2 hours post-exercise.
Conversely, prolonged moderate-intensity exercise progressively lowers blood sugar by increasing glucose uptake into muscles without triggering significant stress hormone release. For people taking diabetes medications, this can occasionally result in hypoglycemia if not properly managed.
Timing and Type Matter
The blood sugar impact of exercise depends on multiple factors: exercise type, intensity, duration, timing relative to meals, current fitness level, and individual metabolic health status. Resistance training builds muscle mass that serves as a glucose “sink,” improving long-term blood sugar control even if individual sessions show temporary elevations.
Rather than obsessing over immediate glucose readings during workouts, focus on the cumulative benefits: improved insulin sensitivity, increased lean muscle mass, better cardiovascular health, and enhanced glucose disposal capacity that manifest over weeks and months of consistent training.
Myth #5: Frequent Small Meals Stabilize Blood Sugar Better 🍽️
The “eat every 2-3 hours to stabilize blood sugar” advice has been repeated so frequently that many accept it as gospel. However, emerging research and clinical experience challenge this conventional wisdom, suggesting that meal frequency is far less important than meal quality and individual metabolic factors.
The theory behind frequent small meals was that constant food intake prevents blood sugar drops and maintains steady glucose levels. In practice, continuously eating—especially carbohydrate-containing foods—keeps insulin levels chronically elevated, potentially contributing to insulin resistance over time.
Recent studies on time-restricted eating and intermittent fasting demonstrate that extending periods between meals actually improves insulin sensitivity, reduces overall glucose levels, and enhances metabolic flexibility—the ability to efficiently switch between burning glucose and fat for fuel.
Individual Responses Vary Significantly
Some people genuinely feel and function better with smaller, more frequent meals, while others thrive on 2-3 larger meals with extended fasting periods overnight. Metabolic health status influences ideal meal timing—those with advanced diabetes and taking certain medications may require more consistent meal schedules to prevent hypoglycemia.
Rather than following one-size-fits-all meal frequency recommendations, pay attention to your individual responses. Stable energy, absence of intense cravings, good sleep quality, and healthy lab markers indicate your eating pattern works for your body, regardless of whether it matches popular advice.
Myth #6: Artificial Sweeteners Don’t Affect Blood Sugar
The assumption that zero-calorie artificial sweeteners provide a “free pass” for blood sugar management oversimplifies their metabolic impact. While these substances don’t directly raise blood glucose levels, mounting evidence suggests they may influence glucose metabolism through alternative pathways.
Research indicates that artificial sweeteners can alter gut microbiome composition, potentially affecting insulin sensitivity and glucose tolerance. Some studies show that despite containing no calories, certain artificial sweeteners trigger insulin release through sweet taste receptors—a phenomenon called cephalic phase insulin response.
Additionally, regular consumption of intensely sweet substances—even non-caloric ones—may perpetuate sweet cravings and preference for hyper-palatable foods, indirectly affecting food choices and blood sugar control.
A Pragmatic Approach to Sweeteners
The evidence isn’t conclusive enough to condemn all artificial sweeteners entirely, but it does warrant a cautious, moderate approach. Using stevia occasionally in coffee differs significantly from consuming multiple diet sodas daily plus artificially sweetened yogurt, protein bars, and desserts.
Consider gradually reducing overall sweetness preference rather than simply substituting artificial sweeteners for sugar. Over time, taste preferences adapt, and foods that once seemed bland become satisfying while previously enjoyable treats taste overwhelmingly sweet.
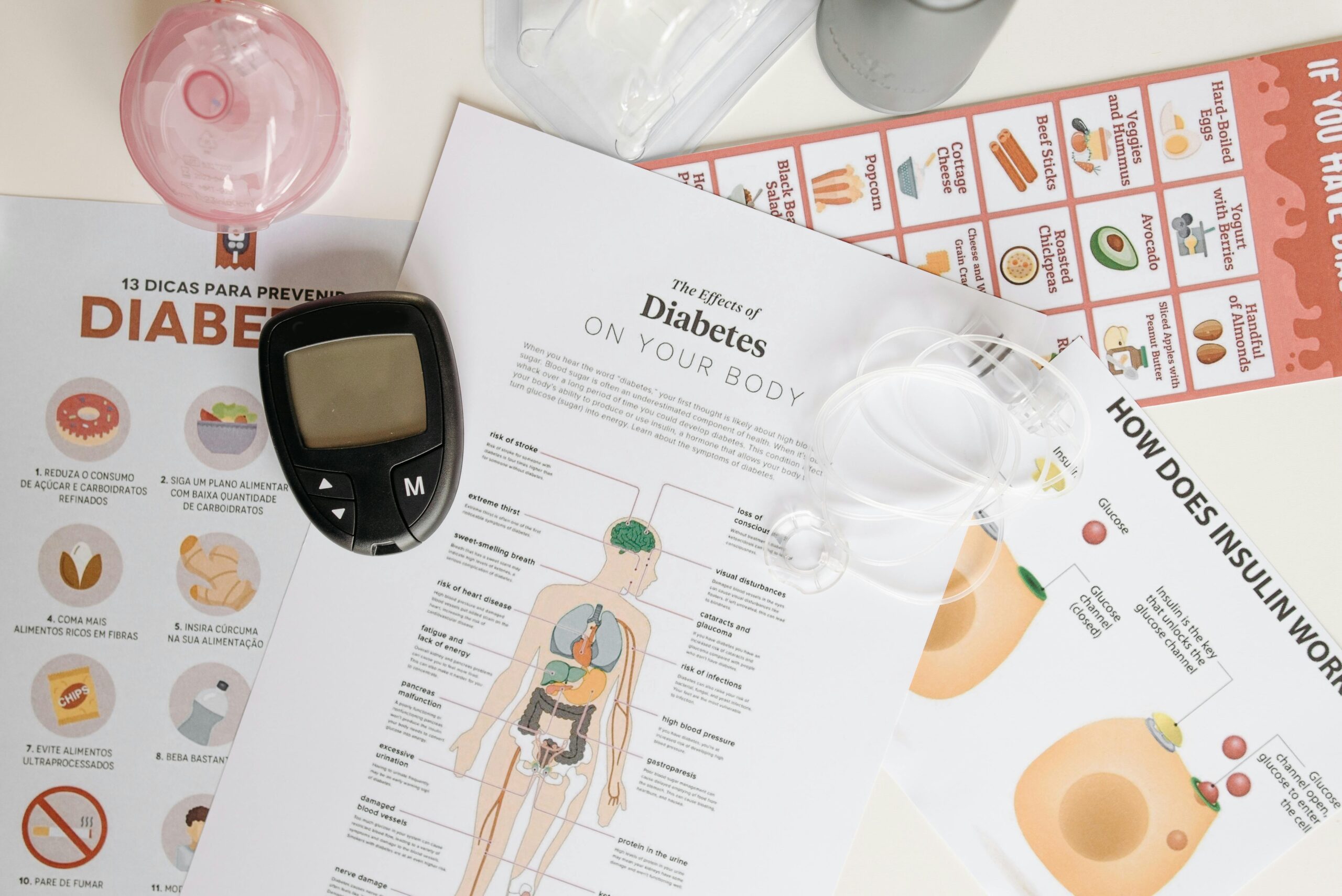
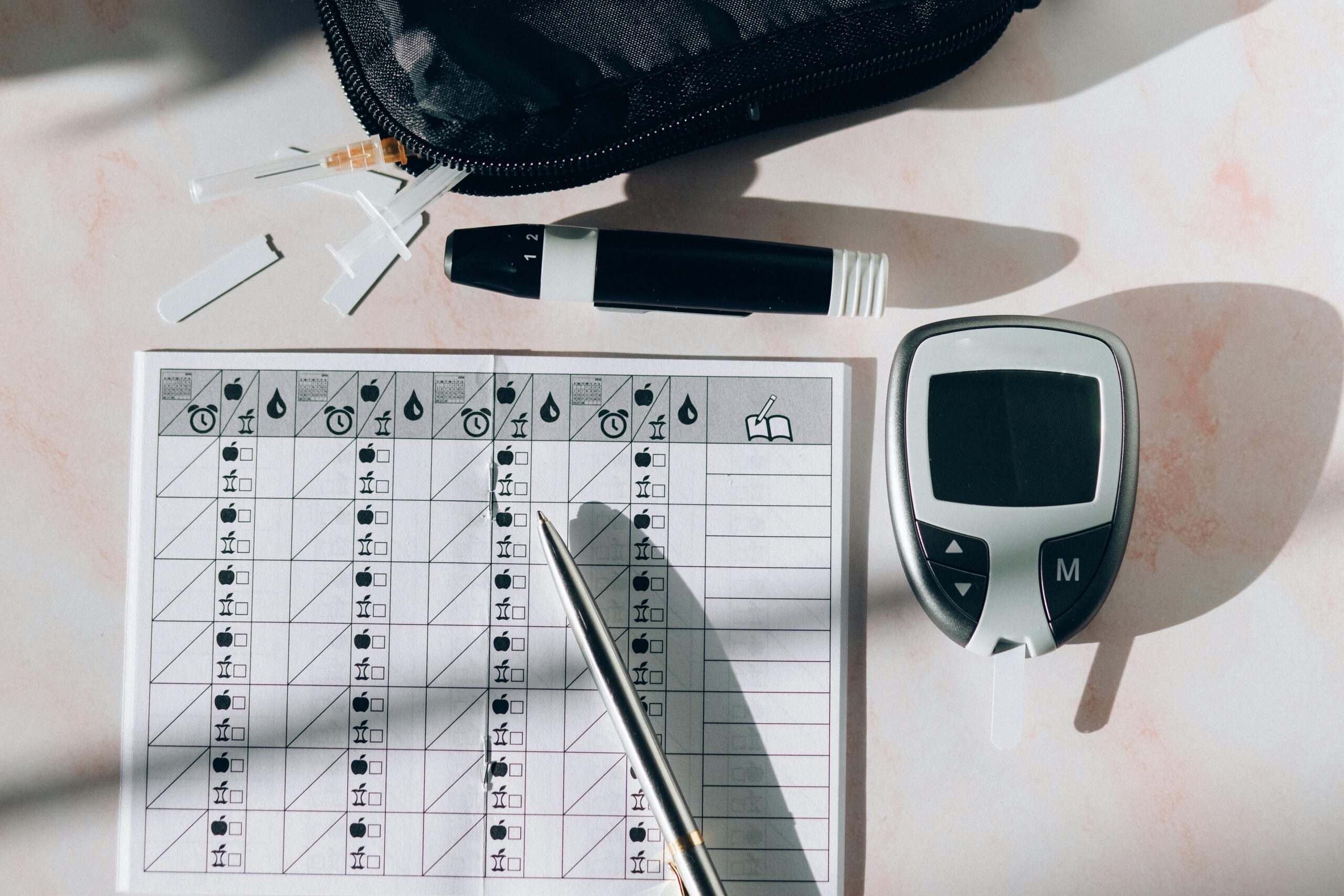
Myth #7: Blood Sugar Testing Is Only for Medication Users 📱
Many people assume that blood glucose testing only serves those taking diabetes medications who need to monitor for dangerous highs or lows. This misconception prevents countless individuals from gaining valuable metabolic insights that could transform their health.
Continuous glucose monitors (CGMs) and even periodic fingerstick testing reveal how your unique body responds to specific foods, meal combinations, exercise timing, sleep deprivation, stress, and other lifestyle factors. This personalized data proves far more valuable than generic dietary advice because metabolic responses vary dramatically between individuals.
Recent research demonstrates that identical foods produce vastly different glucose responses in different people—what spikes your blood sugar might not affect your friend, and vice versa. This explains why universal dietary recommendations often fail; we need personalized approaches based on individual metabolic responses.
Empowerment Through Data
Understanding your personal blood sugar patterns enables informed decisions rather than guesswork. You might discover that rice spikes your glucose but potatoes don’t, that a morning workout stabilizes your levels all day, or that your “healthy” breakfast smoothie causes problematic spikes.
For those interested in tracking blood sugar patterns, various apps help monitor glucose levels and identify trends. While CGMs require prescriptions in many countries, apps that integrate with glucose meters or provide educational resources about blood sugar management can still offer valuable insights into optimizing metabolic health.
Myth #8: Stress and Sleep Don’t Really Matter
The focus on diet and exercise in blood sugar management often overshadows two equally critical factors: stress and sleep. The misconception that you can “eat your way out” of blood sugar problems while neglecting these foundational health pillars sets many people up for frustration and failure. 😴
Chronic stress elevates cortisol, which directly raises blood glucose levels and promotes insulin resistance. Even with perfect diet and exercise, unmanaged stress sabotages blood sugar control. The stress-glucose connection explains why some people see elevated morning readings despite fasting overnight—the dawn phenomenon partly results from cortisol’s natural early morning rise.
Similarly, sleep deprivation dramatically impairs glucose metabolism and insulin sensitivity. Research shows that even a single night of poor sleep increases insulin resistance, elevates next-day blood sugar levels, and intensifies cravings for high-carbohydrate foods. Chronic insufficient sleep increases diabetes risk comparably to obesity.
The Integrated Approach
Sustainable blood sugar management requires addressing diet, movement, stress, and sleep as interconnected rather than isolated factors. Meditation, adequate sleep prioritization, nature exposure, meaningful social connections, and stress-reduction practices aren’t optional luxuries—they’re essential components of metabolic health.
If your blood sugar remains problematic despite dietary improvements, examine your stress levels and sleep quality. Many people discover that addressing these factors produces glucose improvements that diet changes alone couldn’t achieve.
Creating Your Personal Blood Sugar Strategy 🎯
Now that we’ve debunked common myths, how do you create an effective, personalized approach to blood sugar stability? The answer lies in combining evidence-based principles with individual experimentation and honest self-assessment.
Start by focusing on whole, minimally processed foods with an emphasis on vegetables, quality proteins, healthy fats, and fiber-rich carbohydrates. This foundation supports stable glucose levels regardless of specific dietary philosophy—whether low-carb, Mediterranean, plant-based, or another approach.
Incorporate regular physical activity including both aerobic exercise and resistance training. Movement doesn’t require gym memberships or complex routines; walking after meals, taking stairs, gardening, dancing, and playing with children all contribute to improved glucose metabolism.
Prioritize sleep by maintaining consistent schedules, creating dark, cool sleeping environments, and limiting screen exposure before bed. Aim for 7-9 hours nightly, recognizing that sleep is when crucial metabolic restoration occurs.
Develop stress management practices that actually fit your life and preferences. Meditation helps many people, but so do hobbies, time in nature, religious practices, therapy, journaling, or creative pursuits. The best stress management technique is one you’ll actually use consistently.
The Truth About Sustainable Change
Perhaps the most important myth to debunk is that blood sugar management requires perfection or extreme measures. Sustainable metabolic health emerges from consistent, moderate habits maintained over time rather than short-term intensive interventions.
Small improvements compound into significant results. Replacing one daily soda with water, adding a 10-minute walk after dinner, or going to bed 30 minutes earlier may seem insignificant individually, but collectively these changes profoundly impact blood sugar patterns and overall health.
Progress isn’t linear—expect fluctuations, setbacks, and plateaus. What matters is the overall trajectory over weeks, months, and years rather than daily perfection. Self-compassion and realistic expectations prove far more effective than harsh self-criticism and unsustainable perfectionism.
Blood sugar stability fundamentally supports the energy, mental clarity, and physical health that enable you to pursue what matters most in life. By understanding the truth behind common misconceptions, you’re equipped to make informed decisions that genuinely serve your wellbeing rather than following myths that may actually undermine your health goals.
Remember that metabolic health exists on a spectrum, and wherever you currently stand, meaningful improvement is possible through evidence-based lifestyle modifications. The journey toward stable blood sugar isn’t about following rigid rules or achieving perfection—it’s about discovering what works for your unique body and creating sustainable habits that enhance your life quality both now and in the decades ahead. 💪
Toni Santos is a metabolic rhythm researcher and circadian nutrition specialist focusing on the study of blood-sugar oscillation patterns, clock-aligned eating frameworks, and the physiological languages embedded in energy dynamics and restorative sleep. Through an interdisciplinary and data-focused lens, Toni investigates how humanity can decode metabolic balance, vitality, and recovery into the nutritional world — across rhythms, cycles, and optimized routines. His work is grounded in a fascination with nutrition not only as fuel, but as carriers of temporal meaning. From blood-sugar rhythm tracking to energy-curve optimization and clock-aligned meal cycles, Toni uncovers the metabolic and temporal tools through which individuals preserve their relationship with the circadian unknown. With a background in metabolic analytics and circadian nutrition science, Toni blends rhythm analysis with biological research to reveal how meals were used to shape vitality, transmit energy, and encode restorative knowledge. As the creative mind behind montyrax, Toni curates illustrated metabolic maps, speculative rhythm studies, and temporal interpretations that revive the deep biological ties between nutrition, circadian cycles, and forgotten metabolic science. His work is a tribute to: The lost metabolic wisdom of Blood-Sugar Rhythm Tracking Practices The guarded rituals of Clock-Aligned and Circadian Meal Cultivation The physiological presence of Energy-Curve Optimization Rhythms The layered temporal language of Sleep-Compatible Nutrition and Cycles Whether you're a metabolic historian, circadian researcher, or curious gatherer of forgotten rhythm wisdom, Toni invites you to explore the hidden roots of nutritional knowledge — one cycle, one curve, one rhythm at a time.