Blood sugar doesn’t remain constant throughout the day—it rises, falls, and shifts in intricate patterns that can profoundly impact your energy, mood, and long-term health. 🩸
Understanding these daily fluctuations is no longer reserved for diabetics alone. Whether you’re an athlete optimizing performance, a professional battling afternoon energy crashes, or someone simply seeking better health, learning how your body manages glucose rhythms can be transformative. The intricate dance between insulin, cortisol, physical activity, and meal timing creates a unique metabolic signature that influences everything from cognitive function to disease risk.
This comprehensive guide will unlock the mystery behind blood-sugar rhythms, revealing the science-backed strategies that can help you harness these natural fluctuations for optimal vitality and wellness.
The Science Behind Blood-Sugar Oscillations 🔬
Your body maintains blood glucose within a remarkably tight range—typically between 70-100 mg/dL when fasting—through a sophisticated regulatory system. This homeostatic balance involves multiple organs, hormones, and feedback loops working in concert.
The pancreas serves as the primary conductor of this metabolic orchestra. When blood sugar rises after eating, beta cells release insulin, which signals cells to absorb glucose from the bloodstream. Conversely, when levels drop, alpha cells secrete glucagon, prompting the liver to release stored glucose.
However, this system doesn’t operate identically at all hours. Research has revealed that insulin sensitivity—your cells’ responsiveness to insulin—follows a circadian pattern, typically peaking in the morning and declining throughout the day. This means the same meal consumed at breakfast versus dinner can produce dramatically different glycemic responses.
The Circadian Connection to Glucose Metabolism
Your internal biological clock, governed by the suprachiasmatic nucleus in the hypothalamus, doesn’t just regulate sleep-wake cycles. It orchestrates metabolic processes across virtually every cell in your body, including those involved in glucose regulation.
Studies have demonstrated that disrupting circadian rhythms—through shift work, irregular eating patterns, or insufficient sleep—can impair glucose tolerance and increase diabetes risk. The body anticipates food intake at regular times, priming metabolic pathways accordingly. When you eat against your biological clock, this preparation is absent, leading to suboptimal glucose handling.
Mapping Your Daily Glucose Journey 📊
A typical day presents several predictable glucose fluctuation patterns, each influenced by hormonal changes, activity levels, and food intake:
The Dawn Phenomenon: Morning’s Metabolic Awakening
Many people experience elevated fasting glucose in the early morning hours, even without eating. This “dawn phenomenon” results from hormonal surges—particularly cortisol and growth hormone—that occur between 4-8 AM. These hormones trigger the liver to release glucose, preparing your body for the day’s energy demands.
For most individuals, this represents normal physiology. However, in people with diabetes or prediabetes, insufficient insulin response can cause morning glucose to spike excessively, contributing to elevated hemoglobin A1c levels over time.
Post-Meal Peaks: Understanding Glycemic Response
After eating, blood sugar naturally rises. In healthy individuals, glucose typically peaks 60-90 minutes after a meal, reaching approximately 120-140 mg/dL before returning to baseline within two to three hours. The magnitude and duration of this spike depend on several factors:
- The glycemic index and glycemic load of consumed foods
- Fiber content, which slows glucose absorption
- Protein and fat content, which moderate carbohydrate digestion
- Recent physical activity and current insulin sensitivity
- Time of day and circadian metabolic state
- Gut microbiome composition and digestive enzyme activity
Research from personalized nutrition studies reveals remarkable individual variability. Two people eating identical meals can exhibit completely different glucose responses based on their unique metabolic characteristics, gut bacteria, and lifestyle factors.
The Afternoon Slump: Metabolic Midday Mystery
That familiar post-lunch energy dip around 2-3 PM isn’t purely psychological. Several physiological factors converge during this window: declining insulin sensitivity as the day progresses, postprandial glucose fluctuations from lunch, and natural circadian dips in alertness.
This period represents a vulnerable time for poor food choices. When blood sugar drops or becomes unstable, cravings for quick-energy foods intensify, potentially setting off a cycle of glucose spikes and crashes that perpetuates energy instability.
Hormonal Conductors of Glucose Control 🎼
Beyond insulin and glucagon, numerous hormones modulate blood-sugar rhythms throughout the day:
Cortisol: The Stress-Sugar Connection
This stress hormone follows a distinct diurnal pattern, peaking shortly after waking and gradually declining throughout the day. Cortisol raises blood glucose by promoting gluconeogenesis (glucose production from non-carbohydrate sources) and reducing insulin sensitivity.
Chronic stress disrupts this natural cortisol rhythm, leading to persistently elevated levels that contribute to insulin resistance, abdominal fat accumulation, and increased diabetes risk. Managing stress becomes not just a mental health priority but a metabolic imperative.
Melatonin: When Sleep Hormone Meets Metabolism
Recent research has uncovered unexpected connections between melatonin—the “sleep hormone”—and glucose regulation. Melatonin receptors exist on pancreatic beta cells, and genetic variations in these receptors have been linked to type 2 diabetes risk.
Eating late at night, when melatonin levels are elevated, appears to impair glucose tolerance. This finding provides mechanistic support for time-restricted eating approaches that align food intake with circadian biology.
Lifestyle Strategies for Glucose Optimization ⚡
Timing Matters: Chronobiology-Based Eating
Aligning meal timing with your circadian rhythm represents one of the most powerful interventions for glucose stability. Research consistently demonstrates that front-loading calories—consuming larger meals earlier in the day when insulin sensitivity is highest—improves glycemic control compared to evening-heavy eating patterns.
Time-restricted eating, where food consumption is limited to an 8-12 hour window aligned with daylight hours, has shown impressive benefits for glucose regulation, even without caloric restriction. This approach allows extended fasting periods that promote metabolic switching and cellular repair processes.
Movement as Medicine: Exercise Timing and Glucose Control
Physical activity profoundly influences glucose dynamics, but timing dramatically affects its impact. Post-meal walks of just 10-15 minutes can reduce glucose spikes by 20-30%, as contracting muscles absorb glucose independently of insulin through different transport mechanisms.
Morning exercise, particularly before breakfast, enhances fat oxidation and may improve insulin sensitivity throughout the day. However, evening workouts can interfere with sleep quality in some individuals, potentially offsetting metabolic benefits through circadian disruption.
Sleep: The Underestimated Metabolic Regulator
Sleep deprivation—even just one night of insufficient rest—impairs glucose tolerance to a degree comparable to prediabetes. Chronic sleep restriction decreases insulin sensitivity, increases appetite hormones, and disrupts circadian clock genes involved in metabolic regulation.
Prioritizing 7-9 hours of quality sleep, maintaining consistent sleep-wake schedules, and optimizing sleep environment represent foundational interventions for glucose stability that rival many dietary approaches in effectiveness.
Nutritional Strategies for Balanced Blood Sugar 🥗
Macronutrient Composition and Glucose Response
The composition of your meals dramatically influences subsequent glucose patterns. Meals dominated by refined carbohydrates produce rapid spikes followed by reactive crashes, while balanced meals containing protein, healthy fats, and fiber create gentler, more sustained glucose curves.
Protein activates incretin hormones that enhance insulin secretion and promote satiety. Fats slow gastric emptying, moderating the rate of carbohydrate absorption. Fiber, particularly soluble fiber, forms a gel in the digestive tract that buffers glucose absorption and feeds beneficial gut bacteria.
The Unexpected Impact of Meal Sequence
Fascinating research has revealed that the order in which you consume foods within a meal affects glycemic response. Eating vegetables and protein before carbohydrates can reduce post-meal glucose spikes by up to 40% compared to consuming the same foods in reverse order.
This “food sequencing” approach works by pre-loading the digestive system with fiber and nutrients that slow subsequent carbohydrate absorption, creating a more gradual glucose rise without requiring dietary restriction.
Hydration and Glucose Concentration
Adequate hydration plays an often-overlooked role in glucose regulation. Dehydration increases blood glucose concentration mechanically while also impairing insulin secretion. Moreover, elevated blood sugar causes increased urination, potentially creating a dehydration cycle.
Maintaining consistent hydration throughout the day—particularly with water rather than sugary beverages—supports stable glucose levels and optimal metabolic function.
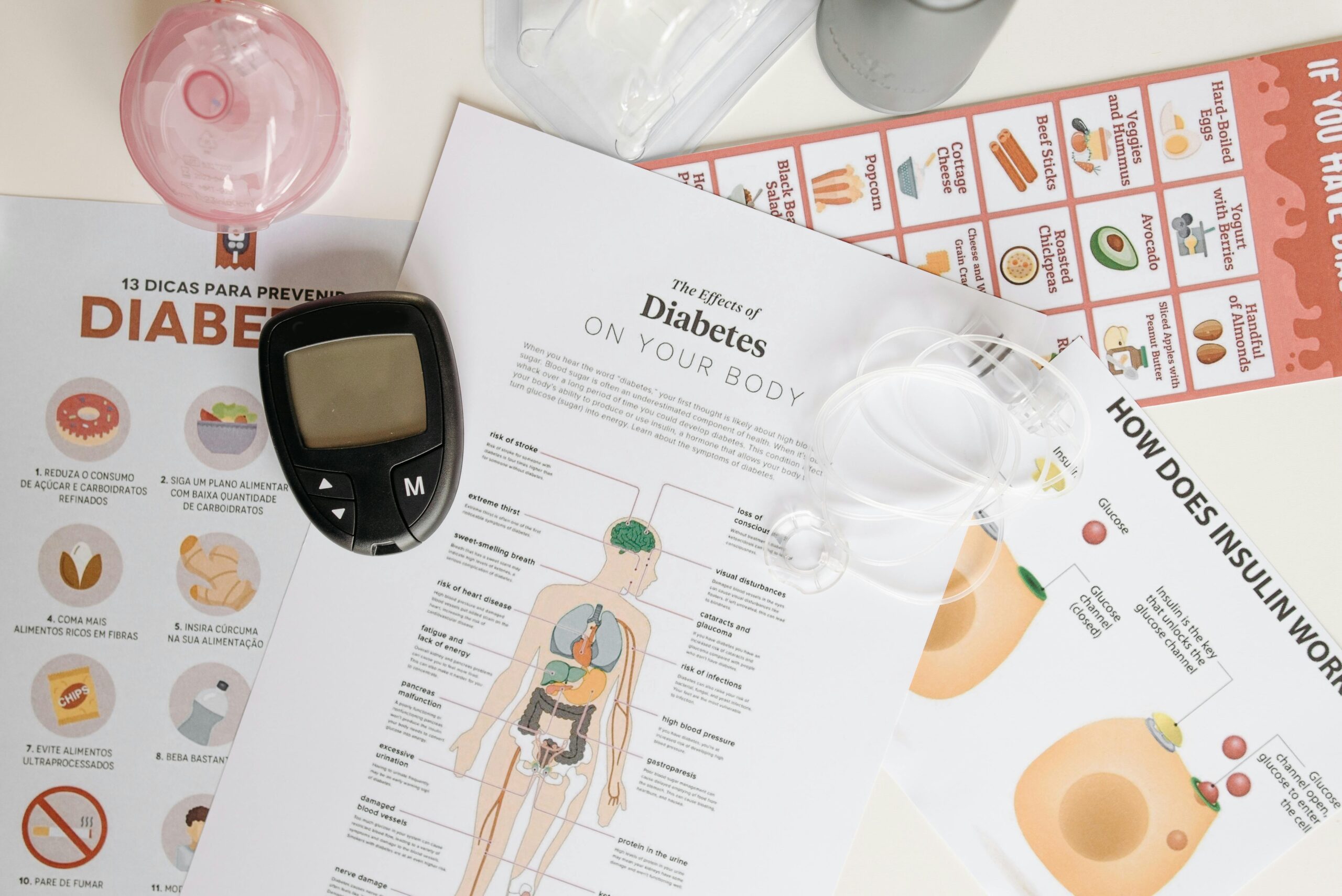
Technology Tools for Glucose Awareness 📱
The democratization of glucose monitoring technology has revolutionized personal metabolic awareness. Continuous glucose monitors (CGMs), once available only to diabetics, now offer health-conscious individuals unprecedented insight into their glucose patterns.
These devices reveal how specific foods, stress episodes, sleep quality, and exercise timing affect your unique glucose rhythms. This biofeedback enables personalized optimization that generic dietary advice cannot provide.
Several smartphone applications now help track glucose patterns, identify trends, and correlate glucose fluctuations with lifestyle factors. These digital tools transform abstract metabolic data into actionable insights for daily decision-making.
When Fluctuations Become Problematic 🚨
Recognizing Dysregulation Patterns
While normal glucose fluctuations reflect healthy metabolic flexibility, certain patterns signal emerging problems. Fasting glucose consistently above 100 mg/dL, post-meal readings exceeding 180 mg/dL, or glucose remaining elevated more than three hours after eating warrant medical evaluation.
Reactive hypoglycemia—blood sugar dropping excessively 2-4 hours after meals—causes shakiness, irritability, and intense cravings. This pattern often indicates insulin oversecretion or early insulin resistance and benefits from dietary modification emphasizing low-glycemic, balanced meals.
The Prediabetes Window: Opportunity for Reversal
Prediabetes affects approximately one in three adults, yet fewer than 20% are aware of their condition. This metabolic state—characterized by fasting glucose of 100-125 mg/dL or hemoglobin A1c of 5.7-6.4%—represents a critical intervention window.
Research demonstrates that lifestyle modifications during the prediabetes stage can prevent or delay progression to type 2 diabetes by 58-71%. The interventions that prove most effective mirror the strategies discussed throughout this article: optimized meal timing, regular physical activity, stress management, and prioritized sleep.
Individual Variation: Your Unique Glucose Signature ✨
Perhaps the most important revelation from recent metabolic research is the profound individual variability in glucose responses. Genetic factors, gut microbiome composition, body composition, fitness level, stress patterns, and sleep quality all contribute to your metabolic fingerprint.
This personalization explains why universal dietary recommendations often fail. The diet that stabilizes one person’s blood sugar might destabilize another’s. Self-experimentation—ideally guided by glucose monitoring and professional support—allows discovery of your optimal metabolic strategy.
Creating Your Personal Glucose Optimization Plan 🎯
Armed with understanding of blood-sugar rhythms, you can design a personalized approach that works with rather than against your biology:
- Establish consistent meal timing aligned with daylight hours
- Front-load calories toward earlier in the day when insulin sensitivity peaks
- Incorporate brief movement sessions after meals to blunt glucose spikes
- Prioritize 7-9 hours of quality sleep with consistent timing
- Build meals around protein, healthy fats, fiber, and non-starchy vegetables
- Experiment with food sequencing—vegetables and protein before starches
- Manage stress through proven techniques like meditation or nature exposure
- Stay consistently hydrated throughout the day
- Consider glucose monitoring to identify your personal patterns and triggers
- Work with healthcare providers when patterns suggest metabolic dysfunction
The Metabolic Mastery Mindset 🧠
Understanding blood-sugar rhythms isn’t about achieving perfection or obsessing over every glucose fluctuation. Rather, it’s about developing metabolic awareness that empowers informed choices aligned with your health goals.
Your body possesses remarkable adaptive capacity. Occasional indulgences, schedule disruptions, or less-than-ideal meals don’t erase the benefits of generally sound metabolic practices. Consistency matters more than perfection, and sustainable approaches outperform rigid protocols that cannot be maintained long-term.
The relationship between glucose stability and overall health extends far beyond diabetes prevention. Stable blood sugar supports sustained energy, cognitive clarity, emotional balance, inflammation reduction, cardiovascular health, and healthy aging. These benefits emerge not from eliminating all glucose fluctuation—which would be impossible and undesirable—but from supporting your body’s natural regulatory mechanisms.

Beyond Glucose: The Bigger Health Picture 🌟
While this article focuses on blood-sugar rhythms, glucose regulation doesn’t exist in isolation. It interconnects with every aspect of metabolism, inflammation, hormonal balance, and cellular function. The strategies that optimize glucose often simultaneously benefit multiple health dimensions.
The circadian alignment that improves glucose handling also enhances sleep quality, immune function, and mental health. The stress management that reduces cortisol-driven glucose elevation also lowers cardiovascular risk and supports cognitive longevity. The movement that buffers post-meal spikes also builds metabolic resilience and functional capacity.
This integration reminds us that health optimization isn’t about isolating individual biomarkers but about supporting the interconnected systems that enable human flourishing. Blood-sugar rhythms provide a measurable window into metabolic health, but the ultimate goal extends beyond any single metric to comprehensive vitality and wellness.
By understanding and working with your body’s natural glucose rhythms rather than fighting against them, you unlock metabolic potential that translates into tangible improvements in how you feel, function, and thrive throughout each day and across your lifespan. The mystery of blood-sugar fluctuations, once decoded, becomes a powerful tool for personalized health optimization that respects your unique biology while leveraging universal metabolic principles.
Toni Santos is a metabolic rhythm researcher and circadian nutrition specialist focusing on the study of blood-sugar oscillation patterns, clock-aligned eating frameworks, and the physiological languages embedded in energy dynamics and restorative sleep. Through an interdisciplinary and data-focused lens, Toni investigates how humanity can decode metabolic balance, vitality, and recovery into the nutritional world — across rhythms, cycles, and optimized routines. His work is grounded in a fascination with nutrition not only as fuel, but as carriers of temporal meaning. From blood-sugar rhythm tracking to energy-curve optimization and clock-aligned meal cycles, Toni uncovers the metabolic and temporal tools through which individuals preserve their relationship with the circadian unknown. With a background in metabolic analytics and circadian nutrition science, Toni blends rhythm analysis with biological research to reveal how meals were used to shape vitality, transmit energy, and encode restorative knowledge. As the creative mind behind montyrax, Toni curates illustrated metabolic maps, speculative rhythm studies, and temporal interpretations that revive the deep biological ties between nutrition, circadian cycles, and forgotten metabolic science. His work is a tribute to: The lost metabolic wisdom of Blood-Sugar Rhythm Tracking Practices The guarded rituals of Clock-Aligned and Circadian Meal Cultivation The physiological presence of Energy-Curve Optimization Rhythms The layered temporal language of Sleep-Compatible Nutrition and Cycles Whether you're a metabolic historian, circadian researcher, or curious gatherer of forgotten rhythm wisdom, Toni invites you to explore the hidden roots of nutritional knowledge — one cycle, one curve, one rhythm at a time.